ISSN 2764-1449 | ISSN (Online) 2764-1430


INTRODUCTION
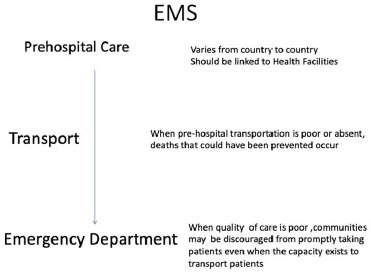
Emergency medicine has long been established as the main medical specialty in Australasia, Canada, Ireland, the United Kingdom and the United States. However, emergency medicine is an interdisciplinary specialty, interdependent of all other clinical disciplines1. According to the EuSEM (European Society of Emergency Medicine), pre-hospital emergency care is an integral part of emergency medicine as the first link in the chain of survival and is available to all European citizens. Pre-hospital emergency care requires a specific set of knowledge and skills from providers, based on knowledge and exceptional experience working in the emergency department 2. Despite different organizations within European countries, the pre-hospital EMS wishes to develop pre-hospital emergency care and ensure the best quality of service throughout Europe (Figure 1).
Emergency department (ED) overcrowding and in particular “access block” potentially represent the greatest threats to the primary mission of emergency care worldwide. The problem is pervasive, large-scale and amounts to a public health emergency with sometimes disastrous consequences. COVID-19 represents a great example of how crowding and blocked access to emergency rooms can be dangerous for pandemic infections3. The main unifying acts for the management of emergencies within the European Union were the creation in 1991 of the common emergency phone call number”112”. In the last 20 years, the number of ED visits double all over the world without explanation with the concept of overcrowding, mainly linked to a shortage of beds.
EMERGENCIES IN DEVELOPED COUNTRIES
The goal of emergency medicine is to stabilize patients who have a life-threatening injury or illness. Unlike preventive medicine or primary care, emergency medical care focuses on providing immediate or urgent medical interventions. It includes two main elements: the medical decision-making and actions necessary to prevent death or disability due to urgent medical conditions, regardless of the patient’s age, sex, location or condition6.
EMERGENCY MEDICAL CARE AND TRANSPORT AROUND THE WORLD
Lack of emergency medical transport is a common barrier to emergency care due to several factors, including the lack of suitable vehicles or the inability to pay for transport services. The consequences of a lack of transportation can be dangerous for patients7,8. Rather than attempting to create a de novo emergency medical care system, the use of established primary care centers could serve as on-site casualty management points for initial assessment.
When a patient’s condition requires resources that a primary care center does not have, they can be transferred to the nearest hospital. The involvement of primary health care centers in the provision of emergency medical care should reduce the risk of district and regional hospitals being overwhelmed with non-emergency cases.
According to WHO data, the main causes of emergencies in the world are medical causes mora than road trafic injuries as in India, China or Turkey9 (Figure 2).
For the majority of EU countries, 112 is the emergency phone number.
In Sweden and Portugal, 112 is the single emergency telephone number. Ambulance dispatch is controlled by a regional dispatch center, which can also coordinate fire and rescue calls (Figure 3).
For emergency calls, particularly in the UK, Sweden, Belgium and Finland, the operator is a technician, nurse or paramedic using intervention protocols. In 30% of European countries, Dispatch Centers don’t have a supervising doctor on the phone. They use a national standard categorization tool from A (life-threatening 25%) to C (non-emergency). The dispatch center in Stockholm is the largest in Europe, almost 60% of pre-hospital EMS use the dispatch center dispatch calls for emergencies, but only 30% have a doctor on the phone. Overall, the number of EMS phone calls continues to grow without an increasing number of ambulances likely related to better medical advice with a doctor on the phone. The management of emergency telephone calls is organized with a Emergency Physician in France, Spain, Portugal and Italy.
There are no studies in Europe that analyze and demonstrate that the regulation system could be more effective if an ambulance driver, nurse, or doctor is on the phone. Nevertheless, a good organization of the “dispatch Center” of the ambulances seems to avoid overcrowding of the emergencies.
EMERGENCY IN THE WORLD
The growth in emergency room activity is also observed in almost all countries in Europe, Asia and North America with multifactorial causes (Figure 4). In Germany, Italy and Spain, emergency services are experiencing an increase in their attendance, but there are no national figures due to the decentralization of their health systems10. Comparative data in Europe on the distribution of doctors per thousand inhabitants shows significant differences from country to country, but with a reduction of nearly 30% in the number of beds in hospitals (see Figure 5). As a corollary, there has been an increase in the number of visits to the emergency room over the past 20 years and the problem of overcrowding has become a daily challenge without universal solutions.
GERMANY:
N of Doctors/inhab: 4.25‰ i.e. +53% in 30 years;
No specialty in MU;
The German system use a liberal medicine that seems better distributed on the territory and better controlled.
• Pre-hospital emergencies, with the regulation of non-medical urgent calls and a significantly variable organization depending on the region,
• Intra-hospital emergencies, which are neither a specialty in their own right nor an independent service.
The German healthcare system has been based on compulsory health insurance since its foundation by Bismarck in 188311.
There are 2,260 hospitals with about 572,000 acute hospitalization beds, corresponding to an average of 7 beds per 1,000 inhabitants in 1998 (figure varying according to the Länder, nevertheless very clearly above the European average which is 4.5)12.
There is no recognized EM specialty in Germany: an emergency medicine sub-specialty with 2 years of additional training (anaesthesia, general medicine, internal medicine, neurology, pediatrics or surgery), including 6 months of training in an intensive care unit, interdisciplinary theoretical courses, 50 outings in medical ambulances under the responsibility of an experienced doctor and a final exam. This qualification is not mandatory to work in emergency medicine.
There are 2 types of emergency physicians.10:
• hospital employees and practice in different specialties (anaesthesia, surgery, internal medicine) they must respond to urgent calls, for which they are not paid if they occur during their working hours at the hospital;
• The other doctors practicing in the ED, better trained, more experienced, more motivated, and paid for each intervention13.
Germany presents a uniform emergency system for each Länder, with legislative provisions regulating the structure of the service, the qualification of the personnel and the financing of the system. The emergency medicine system must be accessible to all citizens. The state can delegate this responsibility in whole or in part to other organizations, such as the fire brigade, the German Red Cross (DRK), including private emergency medicine companies. The emergency rescue service or “Nottfallrettung” and medical transport form a set of secondary prevention health organization13,15. Hospitals organize their emergencies freely, but the majority of emergency rooms correspond to reception areas attached to internal medicine departments, with nurses assigned to the department and doctors from other disciplines taking turns on duty. Patients are sorted upon arrival, according to symptomatologic criteria specific to the service, by an experienced nurse, then referred to the appropriate specialist according to the level of urgency. Senior doctors (“oberartz”) are paid around €4,500/month, assistants (“assistenzartz”, interns after 1 years of training) €3,500/month and first-year interns (“Artz Im Practikum or “AIP”) €1200/month. Guards are paid in addition to salary. Assistants have the same level of responsibility as interns in France. - All doctors are employees under contract. - Doctors work (in theory) 38.5 hours per week.
SPAIN:
• (Sub)Specialty: 1988
• N of Doctors/inhabitant: 3.87‰ (+91% in 30 years)
• Number of emergency physicians: > 8,000 (2021)
Spain has one of the most efficient health systems in the world according to the Bloomberg Health Efficiency Index (2018).
One of the main reasons for this achievement is the Electronic Health Records (EHR) system implemented more than 20 years ago in the country. This system has improved communication between patients and healthcare professionals and helped accelerate research by enhancing the ability to diagnose disease and improving clinical accuracy and outcomes. Another key success factor for the digitalization of healthcare in the country are the many startups that are present there. For example, Doctoralia is a recognized digital platform, born from a Spanish startup, helps around 200 million users a year to find doctors and get appointments in 20 different countries.
General medicine seems better organized, totally public, with health centers and emergency consultations 24 hours a day. But the long waiting times encourage patients to resort too systematically to the emergency room. 2/3 of Spanish population (20 million) call on the emergency services each year with a part that should be taken care of on an ambulatory or primary care.
Emergency room consultations are completely free for patients. There are generally too many doctors in Spain, except in the ED. With 3.4 donors per million deceased inhabitants (28.7 in France), Spain (particularly Barcelona and Madrid) has held the world record for organ donation and grafts for 30 years.
Emergency services funded by hospitals, operating with dedicated staff. Emergencies are separated into 2 distinct concepts: - “urgencias”, corresponding to urgent situations not involving vital risk, - the “emergencias”, where the vital risk is committed.
General practitioners have a legal obligation to perform night shifts, on Sundays and on public holidays, but in this obligation is not respected in large cities.
The organization of prehospital EMS have 4 types of ambulances, all belonging to the regional health service:
• “Heavy” ambulance with medical support, carrying 1 doctor, 1 nurse, and 2 technicians;
• Rapid Intervention Vehicle (VIR), transporting 1 doctor, 1 nurse and 1 technician
• Home care unit or “Unidad d’Attencion Domicilaria (UAD)” for “urgencias”, transport a doctor or nurse with a technician;
• “Light” ambulances or basic support, 2 technicians.
There is no university specialty in emergency medicine in Spain, the doctors working in the emergency system, estimated > 10,000, are family generalists who have most often followed additional training (14). Senior doctors work around 52 hours a week According to the Collegiate Medical Organization (OMC), in the next ten years, 40% of employees in the Spanish public health system will retire. However, the number of positions offered for the various competitions is insufficient and the working conditions are unfavorable (low salary, fixed-term contract) in particular for the recruitment of emergency physicians216.
ITALY
N of Doctors/inhabitant: 3.98‰ (-15% in 30 years)
N Emergency physicians: 3,000 (2021)
The Italian health system is close to the UK National Health System (NHS) but organized by region17.
Emergency medicine has been a medical specialty since 2008: it corresponds to a specific 3-year training course, accessible only to medical specialists (mainly anesthesiologists, resuscitators and cardiologists).
Consumerism is emerging in emergency departments, as well as issues of violence, both in emergency departments and during pre-hospital interventions. Health policies in recent years have reduced the number of acute hospitalization beds in medicine, resulting in the overwhelmed emergency services18.
Pre-hospital emergencies run with a single call number linked to the police but independent of the fire brigade. The emergency call centers depend on the hospital with specialized nurses and doctors.
Hospital emergencies do not have a uniform organization :the triage is organized by hospitalization decision support protocols. Unscheduled ambulatory care seems to be failing with incompetent and overloaded health centers, and paying city medicine for patients without complementary insurance, creating a 2-speed medicine.
The tenured doctors are salaried civil servants belonging to a single body.
The average gross monthly salary of a head of department is €4,500, and €2,000 for a simple senior manager.
The average salary of an emergency physician is around €2,500 /month.
Interns are paid by the university around €700/month.
UK (UNITED KINGDOM)
• Speciality: 1972
• N Doctors/inhabitant: 2.80‰ (+251% in 60 years)
• Number of emergency physicians: 1632
The UK pioneered the creation of the specialty of emergency medicine in the world with its formal establishment in 1972. The health system, NHS in order to regulate the overcrowding of emergency departments (A&E) called “corridors of shame” was illustrated by a radical decision in the 2000s. The NHS having decided to financially penalize hospitals that did not respect the 4-hour rule (“4 hours target”) total management (entrance exit) for any patient who presents to the emergency room. This financial penalty was very effective in forcing the entire hospital to organize patient admissions from the emergency room, but inevitably led to failures and overflows: long waiting time for ambulances in front of the A&E319. The emergency physicians subsequently called for a 6-hour rule with no effect on the reduction in A&E waiting times and the situation was notably exacerbated during the COVID pandemic20.
SWEDEN:
Speciality: 2002
N of Doctors/inhabitant: 3.98‰ + 298% in 60 years
Special features: Person Centered Care mobile geriatric teams
The Swedish healthcare system is organized into three levels: national, regional and local.
The Health and Medical Services Act clarifies that responsibility for ensuring that everyone living in Sweden has access to good health care rests with county councils/regions and municipalities. Therefore, the type of health services available may vary. Full emergency services are located in tertiary care hospitals and most local county hospitals and operate 24 /7. emphasis was placed on the mobile emergency services (ambulances) and the pre-hospital EMS provided by these mobile teams. In an emergency, dial 112 for police, fire department or ambulance. At the same time, there is a move towards the use of mobile emergency EMT, made up of different clinical skills and carrying out home visits, in particular for people who have greater care needs, such as the elderly and people with chronic illnesses.
Overwhelmed ED, shortage of doctors: these constraints have pushed the goverment to innovate to provide better care. Cost effective telemedicine with its northern regions sparsely populated and buried under snow during the long winter months, Sweden has embarked in particular on telemedicine. In Gothenburg, the dermatologist John Paoli has developed an application allowing general practitioners to obtain, by a simple photo taken on a smartphone, the diagnosis of the hospital dermatologist on the dangerousness of an ugly mole. His invention, which received the Swedish Innovation Award in 2013, has already been adopted by 20 regional health centers. Tested on two groups of some 800 patients, it allowed much faster treatment of melanoma cases (nine days instead of thirty-five), avoiding 20% of unnecessary visits to the hospital. A gain of 10 million euros for the community. Another recipe from which other countries could draw inspiration: Person Centered Care, care centered on the staff.
The improvement, qualitative and financial, is obvious: satisfaction rate up sharply and length of stay (LOS) reduced by 25% in six years. With > 25 Million visits/year (3 visits/year for 1 person), the organization of emergency services in Sweden varies according to the type of hospital. In general, in large university hospitals, patients are sorted according to the nature of their complaint: medical or surgical. Pediatric, obstetrics and gynecology, ENT, and ophthalmology patients are all triaged and treated in separate departments that are not associated with the main emergency department. Emergencies are not always considered and manage the input of patients to hospitals 24 hours a day, without being able to control admissions and discharges (ouput), inevitably leading to the accumulation of patients in the emergency room, leading to a lack of security, a bad working environment.
Therefore, Swedish emergency care needs to improve collaboration with other actors, both inside and outside the hospital, such as health care and community care services. Many patients might prefer to seek care at home rather than in an UAS. To a greater extent, some patients could be admitted directly to the services.
CHINA, HONG KONG VIET NAM, SINGAPORE
• Specialty: 1997 (HK), 1984 (Sing) 2010 (Vietnam)
• N of Doctors/inhabitant: 1.98‰ (Ch), 2.3 (Sing) 52,000 doctors 0.83‰ (VN) + 244% in 40 years
• Number of emergency workers: 40,000 (Ch) 212 (Sing)
• System: “ED of internal Medicine”
While emergency medicine is developing in most Asian countries, it can be considered that the development is developing favorably in China and in particular in large cities such as Shenzhen or Hong Kong.
Vietnam has developed private hospital structures for 15 years, allowing foreign capital to be invested and doctors to be recruited based on the wealthy Vietnamese population (or tourists) and allowing reinvestment in the development of hospital structures after 10 years of ‘use. The large volumes of patients presenting to emergencies, particularly in China, are particularly organized and it is therefore curious to see that the young Chinese population resorts to safety emergencies and believes more in modern medicine rather than traditional medicine.
The waiting rooms had to show original organization to combine a young population in a seated position with its magical infusion. Emergency medicine has made great strides in Singapore. It is now a recognized medical specialty with a growing pool of trained physicians and established structured training programs. Emergency medicine in Singapore still faces many challenges, with a marked improvement in the level of emergency patient care as Singapore enters the third millennium.
EMIRATES, DUBAI
• Speciality: 2004
• N of Doctors/inhabitant: 2.53
• Number of emergency physicians 1.93
• High performance system
• Features: 75% minor pb EMS managed by Police.
Emergency medicine was recognized as a specialty in the United Arab Emirates (UAE) in 2004. In this short time, emergency medicine has established itself and grown rapidly in the UAE. Large, well-equipped emergency departments are usually located in public hospitals, some of which operate as regional trauma centers. Most large emergency departments are staffed by physicians trained in medicine or surgery, with board-certified emergency physicians serving as consultants overseeing care. Pre-hospital care and emergency medical services (EMS) operate under the auspices of the police department21. Standard protocols have been established for paramedic certification, triage and destination decisions. Most ambulances offer Basic Life Support (BLS/Type 2) with a growing minority offering Advanced Life Support (ALS/Type 3). The medical residency programs were established 5 years ago and form the basis of training specialists in emergency medicine for the UAE. This article describes the full spectrum of emergency medicine in the UAE: pre-hospital care, EMS, inpatient emergency care, emergency medicine training and disaster preparedness. We hope that our experience, understanding of the challenges facing the specialty, and anticipated future directions will be important to others advancing emergency medicine in their region and around the world21.
US:
• Speciality: 1972
• N of Doctors/inhabitant: 2.61‰
• Number of emergency physicians: 48,835
• System • Peculiarities: Chicago > 20 Firearm Wounds/d
With the creation of the specialty of emergency medicine in 1972, the United States experienced a low period 20 years ago with a disaffection of the specialty of emergency medicine. Thanks to an active recruitment campaign and no doubt probably thanks to the TV show «ER» (from Michael Crichton) in the 1995, the specialty of emergency medicine in the United States is one of the 3 famous speciality by students. in medicine. Attractive, this specialty has become more feminized with work rotation schedules generally 3 shifts per week.
Currently, 3 emergency medicine companies dominate in the United States the SAEM ACEP and AAEM.
The training of young doctors is developed through comprehensive programs integrating simulation22.
There is no Virtually no experience of pre-hospital medicine in the United States, but feedback from the Boston attacks in Las Vegas has made it possible to develop pre-hospital medicine programs based on disaster medicine.
In 1999, the Accreditation Council for Higher Medical Education (ACGME) identified six general competencies as the basic educational objectives required by all training programs for their residents. A consensus workshop held at the 2006 Council of Emergency Medicine Residency Directors (CORD) «Best Practices» conference identified specific measures for five of the six skills in emergency medicine - interpersonal communication skills, patient care, learning based on practice, professionalism, and systems - based on practice (medical knowledge has been excluded).
EMERGENCIES IN THE PACIFIC: AUSTRALIA AND NEW ZEALAND
• Speciality: 1993 (Aus) 1995 (NZ)
• N of Doctors/inhabitant: 3.68‰ (Aus, NZ)
• Number of emergency physicians: 1761 (Aus) 225 (NZ)
• Paramedics base system
Paramedic services in Australia and New Zealand (Australasia) share many characteristics, with both offering versions of the Anglo-American emergency medical response system. The main difference between the two countries is in their sources of funding, with Australian paramedic services generally receiving more government funding than those in New Zealand. Both countries offer a range of services that use a mix of volunteer and professional staff and employ state-of-the-art communication and medical technologies to provide high-level clinical services. Like other high-income countries, they face the challenge of increased use associated with aging populations. Both countries are adapting to this by expanding their response models from a focus on emergency medical response to providing a mobile health service that will see the emergence of more paramedical roles. These emerging models challenge the fundamental missions of paramedic services, as well as the professional identity of paramedics.
The development of the Anglo-Saxon or European model of MU training Emergency Medicine Education initiatives are increasingly developed globally through national and international EM organizations.
Lack of resources and funding capacity in some countries may hamper the development of specialties.
The continued growth of the specialty in these countries requires an understanding of their health priorities and the global health and development agencies that often help these countries support the health sector. Emergency medicine residency programs address the need for physicians trained in emergency medicine in emergency departments. The Accreditation Council for Higher Medical Education (ACGME) Residency Review Committee ensures that all programs have a structured curriculum that includes both didactic and bedside teaching, as well as structured methods of assessment of residents and faculty. There are three- and four-year training formats for emergency medicine in the United States. In Europe, the EUSEM advocates a 4-5 year training in Emergency Medicine with a curriculum (EBEEM).
OVERCROWDING: A FATALITY FOR THE EMERGENCIES OF THE 21ST CENTURY?
Overcrowding is frequently described in terms of the “input-throughput-output” model by Asplin et al25.
A systematic review by Morley et al. to primary care 23,24,25 which has led to an increase in low acuity presentations,23,25 increased use of emergency departments by the elderly and those with complex conditions,26,27,28 and an overall increase in demand for emergency services.29 Several types of UAS models can be described according to the resources of the different countries30 in an attempt to remedy the use of patients in the emergency room (Figure 6).
SCOOP AND RUN VS STAY AND PLAY
Two major models of emergency care delivery exist today in Europe: the Anglo-American model and the Franco-German model. A majority (63%) of European countries have a pre-hospital EM system (EMS) managed by trained emergency physicians (Figure 7). Various northern European countries use the paramedical system and the pre-hospital EMS is partly managed by doctors (33%) or technicians. Most countries developing new emergency care systems follow the Anglo-American model. In the UK, the turnaround time is reduced from 8 minutes to 20 minutes with Basic Life Support (BLS) sustaining ambulances or Advance Life Support (ALS) ambulances with 7000 paramedics trained (2 years) in the skills of emergency or NHS ambulance service (Figure 8 and 9). In the immediate care plan, some doctors trained in pre-hospital emergency medicine can intervene on site, in helicopter-borne interventions (HEMS) in the UK or Australia. However, the pre-hospital medicalization system may delay the patient’s arrival time at the emergency department.
The experience of Princess Diana’s accident in 1997 had triggered a heavy controversy on the medicalization of pre-hospital relief and the French SAMU model.
However, there are few studies comparing the Franco-German vs Anglo-American models of emergency care.
There are no morbidity/mortality studies to assess the paramedical system.
In the absence of reliable studies comparing the 2 systems «scoop and run» (renamed «load and go») and «stay and play» («stay and stabilize»), the analysis of pre-hospital systems in the world seems above all to be organized at the level of the management of appropriate medical or traumatic emergencies.
Thus, as much the coronary emergency seems favorable to early medicalization to direct the patient as soon as possible to the catheterization room, as much penetrating trauma (stabbing or shooting) require rapid transport to the Trauma Center as US, Israeli ,UK emergency services working with surgical teams and trauma surgeons.
We must nevertheless consider that a combination of the 2 systems with a trained medical team making quick decisions to direct the patient to the right place “stay, stabilize, load and go” would be the best attitude.
The French SAMU pre-hospital system, has demonstrated its expertise in particular in the management of COVID and in particular in long-distance (plane or train)medical transport, shows that this expertise remains expensive and few countries, including America.
The SAMU model in the world?
The dispatchof urgent calls is medicalized in Spain, Italy, Portugal and France.
The technician dispatcher receive urgent calls on the nature and reason for the call.
Regulating physicians are trained in emergency medicine. In Germany, it is “medical emergency technicians” who decide to send a doctor on site. These technicians have undergone validated two-year training (80 hours of theoretical training in regulation and compulsory regular participation in field rescue) can join an emergency doctor if necessary. Thus several French SAMU15 are in America (Guadeloupe, Guyana, Martinique), in Pacific Ocean (Tahiti,New Caledonia ) or in Reunion or Mauritius.
The French SAMU model exists in several Maghreb countries (Algeria, Morocco, Tunisia) as well as in Africa (Benin Ivory Coast, Gabon).
REWARD: TURKEY
• Speciality: 1993
• N of Doctors/inhabitant: 1.85‰
• Number of emergency physicians 1546
• World record system Emergency passages > 2000/day
• Features: 45% violence
With a number of visits of around 1,000 to 2,000 emergency patients over 24 hours in Istanbul, where Ankara Turkey holds the record for the number of emergency patients.
The emergency organization combines a system of paramedics and doctors are trained in all areas of pre-hospital and hospital emergency medicine, particularly in disaster medicine.
Turkish universities are developing teaching models based on American universities.
Despite its relatively short history, emergency medicine residency training in Turkey has developed rapidly in order to meet the demand for such services.
The very first step in the development of emergency medicine residency programs began with the efforts of emergency physician John Fowler, a native of the United States, where emergency medicine was born, following his invitation to join the service department of Dokuz Eylul University Hospital (Izmir, Turkey) in 199031.
A MODEL OF ORGANIZATION - DENMARK:
• Speciality: 2018
• N of Doctors/inhabitant: 4.01‰
• Health system based on MG
• Special features: patients no longer have to go to the emergency room on their own.
In Denmark, patients no longer have to go to the emergency room on their own Since 2014, residents of the Copenhagen area have had to call the emergency number instead of going directly to the hospital in the event of illness or injury. In the rest of the country, it is the general practitioners who organize themselves to guide patients day and night. A model that has relieved emergency services and inspires the French government bogged down in the hospital crisis. But who remains perfectible and under pressure. Today, Danes are no longer supposed to go to the hospital on their own initiative. Faced with the same lack of resources and saturated hospital emergencies, in 2007 the State, which devotes 10.4% of its GDP to health432, spent nearly 6 billion euros over ten years in its hospital transformation plan. The regions, responsible for primary care and emergencies, had to find solutions to compensate for the closure of hospitals. Go to the emergency room... by appointment On the front line, general practitioners have become the cornerstone of the Danish health system533. Patients must go through a doctor before going to the emergency room. “Outside the opening hours of the practices, the general practitioners take turns answering a medical assistance number and, if necessary, receive consultations or visit patients. more serious», explains Jonatan Schloss, president of the Organization of General Practitioners. Denmark is recognized as the “sweet spot” for innovation32.33. Denmark was a pioneer in telehealth, and today e-health is established, becoming a success. Every Danish patient enjoys the benefits of an electronic health record that he and his doctor can access. In addition, many digital services encourage patients to be more proactive in decisions about their health and improve health outcomes. For example, the Telecare North project implemented home care monitoring for patients with COPD or psychiatric conditions32,33. health. According to The health care in Denmark (2008), this project improved the quality of life of patients and reduced the number of hospitalizations by 11%32,33.
Thanks to their digital health strategy, Danish hospitals have reduced the number of outpatient consultations by 75%.
CONCLUSION:
The organization of pre-hospital and hospital emergency services varies from one country to another and in particular has been adapted to the typology of patients.
The use of ED, whether organized by medicalization of the call or by paramedics, does not offer an ideal prospect, because the overcrowding proble remains in almost all countries with multifactorial causes.
The world record for the number of ED visits remains in Turkey.
Apart from the Danish model based on education of the population and an organization based on general medicine, no other model has been developed to better organize the use of emergencies.
The pre-hospital model of the French SAMU remains a costly and expensive system and therefore difficult to transpose in countries with low resources. Apart from the disaster medicine situations of terrorist attacks or COVID crises where the expertise of prehospital medicine of the French SAMU has been recognized, the majority of Anglo-Saxon countries continue to try to develop emergency medicine with multiple patient triage models based on resources. Emergency medicine training based on the Anglo-Saxon model has developed little by little35-39. In Europe, a 4-5 year curriculum has been proposed by the European Society for Emergency Medicine (EUSEM) which will no doubt allow in the future to practice in all the structures of the European Union.
REFERENCES
1. Garel P, Notarangelo I. Hospitals in Europe: Healthcare data [Internet]. HOPE. 2020 [cited 2022 Jan 19]. p. 1–19. Available from: https://hospitalhealthcare.com/latest-issue-2018/hope-2018/hospitals-in-europe-healthcare-data-9/
2. European Curriculum For Emergency Medicine. A document of the EuSEM Task Force on Curriculum approved by the Council and Federation National Societies of the European Society for Emergency Medicine, and by the UEMS Multidisciplinary Joint Committee on Emergency Medicine, and endorsed by the Council of UEMS at their plenary meeting in Brussels on 25 April 2009
3. Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, Bernhard M, Bertini A, Gries A, Ferrandiz S, Kumar VA, Harjola VP, Hogan B, Madsen B, Mason S, Ohlén G, Rainer T, Rathlev N, Revue E, Richardson D, Sattarian M, Schull MJ. International perspectives on emergency department crowding. Acad Emerg Med. 2011 Dec;18(12):1358-70. doi: 10.1111/j.1553-2712.2011.01235.x. PMID: 22168200
4. Baubeau D.,Les passages aux urgences de 1990 à 1998: une demande croissante de soins non programmés, Direction de la Recherche des Etudes de l’Evaluation et des Statistiques, Etudes et Résultats n° 72, juillet 2000.
5. Chanteloup M. Et Gadel G., Les appels d’urgence au centre 15 en 1997, Direction de la Recherche des Etudes de l’Evaluation et des Statistiques, Etudes et Résultats n° 55, mars 2000.
6. Emergency medical care in developing countries: is it worthwhile? Junaid A. Razzak & Arthur L. Kellermann. Bull World Health Organ 2002;80(11):900-5. Epub 2002 Dec 3.
7. Sodemann M. Jakobsen MS. Molbak K, Alvarenga IC, Aaby P. High mortality despite good care-seeking behaviour: a community study of childhood deaths in Guinea-Bissau. Bulletin of the World Health Organization 1997; 75:205-12.
8. Geefjhysen CJ, Isa AR, Hashim M, Barnes A. Malaysian antenatal risk coding and the outcome of pregnancy. Journal of Obstetrics and Gynecological Research 1998;24:13-20.
9. Verghese M, Mohan P. When someone is hurt. A first-aid guide for lay persons and community workers. New Delhi: Other Media Communications; 1998.
10. Etude de l’organisation des differents systemes d’urgence dans cinq pays europeens : la France, L’Allemagne, l’Espagne, l’Italie et le Portugal. These : Marielle CHODOSAS 1995
11. Duriez M. Et Lequet-Slama D., Les systèmes de santé en Europe, collection Que Sais-je? , puf, 3343, mai 1998.
12. Hassenteufel P., : Allemagne, particularisme et régulation professionnelle, Revue PRATIQUES, avril 2002, 17, 14-16.
13. Verite-Usener E., Analyse comparée des systèmes de santé français et allemand à travers la prise en charge pré-hospitalière des urgences, Ecole Nationale de Santé Publique, décembre 1993.
14. Alvarez Fernandez J.A. : Formacion especializada en medicina de emergencias, Med.Clin (Barcelona), Octobre 1995, 105, 11 : 436-437.
15. l’Allemagne se convertit au budget global, Décision Santé, 31 octobre 1999, n° 150,15.
16. Castro NR. Médicos españoles, mayores y sin recambio. ABC Sociedad [Internet]. 2017;1–2. Available from: https://www.abc.es/sociedad/abci-medicos-espanoles-mayores-y-sin-recambio-201711072215_noticia.html
17. European Observatory On Health Care Systems: Health Care System in Transition, Italy, 2001.
18. Ponassi A.G. et al.: Analysis of 1930 bedbridden patients in the internal medical sector of the emergency departement of a large city hospital : appropriate and non-appropriate admission, European Journal of Emergency medicine, 1999, 6, 55-60.
19. NHS. When to go to A&E [Internet]. NHS Services. 2019 [cited 2022 Jan 19]. p. 1–3. Available from: https://www.nhs.uk/nhs-services/urgent-and-emergency-care-services/when-to-go-to-ae/
20. Michael E. Reschen, Jordan Bowen, Alex Novak, Matthew Giles, Sudhir Singh, Daniel Lasserson & Christopher A. O’Callaghan. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emergency Medicine volume 21, Article number: 143 (2021) `
21. Fares et al. International Journal of Emergency Medicine 2014, 7:4 http://www.intjem.com/content/7/1/4
22. The Practice of Emergency Medicine/Original Research National Study of the Emergency Physician Workforce, 2020 Christopher L. Bennett, MD, MA; Ashley F. Sullivan, MS, MPH; Adit A. Ginde, MD, MPH; John Rogers, MD; Janice A. Espinola, MPH; Carson E. Clay, BA; Carlos A. Camargo, Jr, MD, DrPH*
23. Pines J, Pollack C, Diercks D, et al. The Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients with Chest Pain. Acad Emerg Med. 2009;16(7):617-625.
24. Bernstein S, Aronsky D, Duseja R, et al. The Effect of Emergency Department Crowding on Clinically Oriented Outcomes. Acad Emerg Med. 2009;16(1):1-10.
25. Boudi Z, Lauque D, Alsabri M, et al. Association between boarding in the emergency department and in-hospital mortality: A systematic review. PLoS ONE. 2020;15(4):e0231253.
25. bis Innes G, Sivilotti M, Ovens H, et al. Emergency overcrowding and access block: A smaller problem than we think. CJEM. 2018;21(2):177-185.
26. Forero R, McCarthy S, Hillman K. Access block and emergency department overcrowding. Crit Care. 2011;15(2):216.
27. Khanna S, Boyle J, Good N, et al. Unravelling relationships: Hospital occupancy levels, discharge timing and emergency department access block. Emerg Med Australas. 2012;24(5):510-517.
28. FitzGerald G, Jelinek G, Scott D, et al. Emergency department triage revisited. Emerg Med J. 2010;27(2):86-92.
29. Sprivulis P, Da Silva J, Jacobs I, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184(12):616-616.
30. Steptoe et al. International Journal of Emergency Medicine 2011, 4:42
31. Basar Cander. EPAT ATUDER. Turkey EM Journey.
32. OCDE Données. Dépenses de santé. OCDE Données [Internet]. 2021. [cited 2022 Jan 19];1–5. Available from: https://data.oecd.org/fr/healthres/depenses-de-sante.html
33. Foucaud I de. À Strasbourg, ces médecins soulagent le Samu et les urgences - Challenges. Challenges [Internet]. 2019 [cited 2022 Jan 19];1–4. Available from: https://www.challenges.fr/entreprise/sante-et-pharmacie/a-strasbourg-ces-medecins-soulagent-le-samu-et-les-urgences_657135
34. Affleck A, Parks P, Drummond A, et al. Emergency department overcrowding and access block. CJEM. 2013;15(06):359-370.
35. The Foundation Programme Committee of the Academy of Medical Royal Colleges. Curriculum for the Foundation Years in Post Graduate Education and Training. Academy of Medical Royal Colleges. Available at: http://www.dh.gov.uk/prod_consum_dh/ groups/dh_digitalassets/@dh/@en/documents/digitalasset/ dh_4107696.pdf. Accessed February 22, 2009.
36. Liaison Committee on Medical Education. LCME Accreditation Standards (with annotations). Liaison Committee on Medical Education June 2008. Available at: http://www.lcme.org/func- tionslist.htm. Accessed February 22 2009.
37. Frank JR. The CanMEDS 2005 Physician Competency Frame- work. Better Standard, Better Physicians, Better Care. The Royal College of Physicians and Surgeons of Canada. (Accessed March 1, 2009).
38. Manthey DE, Coates WC, Ander DS, Ankel FK, Blumstein H, Christopher TA, et al. Report of the Task Force on National Fourth Year Medical Student Emergency Medicine Curriculum Guide. Ann Emerg Med 2006;47(3):e1-7.
39. Hockberger RS, Binder LS, Chisholm CD, Cushman JT, Hayden SR, Sklar DP, et al. The model of the clinical practice of emergency medicine: a 2-year update. Ann Emerg Med 2005;45(6):659-74. Chapman DM, Hayden S, Sanders AB, Binder LS, Chinnis A, Corrigan K, et al. Integrating the Accreditation Council for Graduate Medical Education Core competencies into the model of the clinical practice of emergency medicine. Ann Emerg Med 2004;43(6):756-69.